Summary
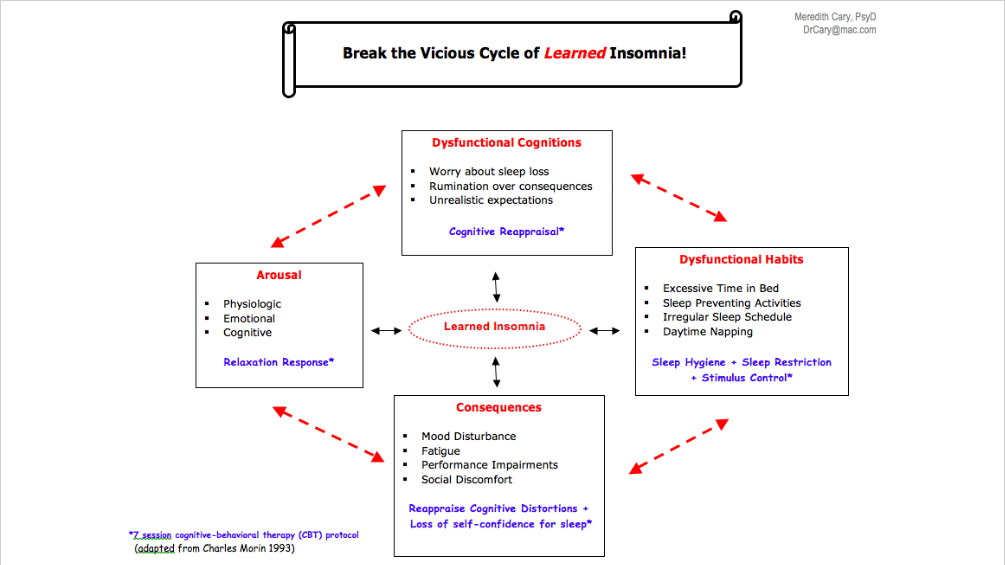
Ads say, “Ask your doctor” for a pill. But, in fact, sleep specialists say that Cognitive Behavioral Therapy for Insomnia (CBT-I) is the FIRST step to take … before any kind of medication.
OnAir Post: CBT-I for Insomnia
About
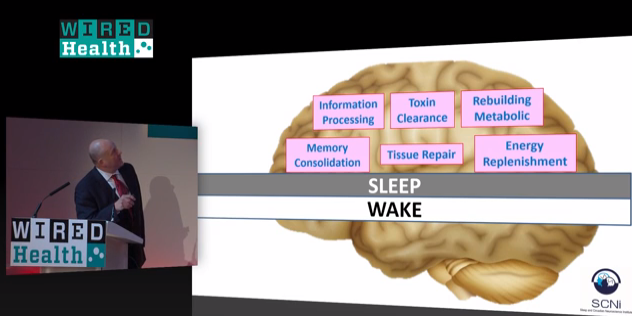
How much sleep do you need?
Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion
Nathaniel F. Watson et al
Sleep Research Society | 2015
Consensus Statement
Adults should sleep 7 or more hours per night on a regular basis to promote optimal health.
The American College of Physicians Recommendation
Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians
Amir Qaseem, MD et al
Annals of Internal Medicine | July 19, 2016
What does CBT-I look like?
This video, produced by psychologists – CBT-I specialists – realistically explains (and shows) the most essential parts of what to expect in CBT-I treatment.
The sleep diary
DOWNLOAD the Sleep Diary + the Instructions here!
The consensus sleep diary: standardizing prospective sleep self-monitoring
Carney, CE et al
Sleep | Sleep Research Society | Volume 35 Issue 02
Abstract
Study Objectives:
To present an expert consensus, standardized, patient-informed sleep diary.
Conclusions:
The Consensus Sleep Diary was the result of collaborations with insomnia experts and potential users. The adoption of a standard sleep diary for insomnia will facilitate comparisons across studies and advance the field. The proposed diary is intended as a living document which still needs to be tested, refined, and validated.
Does computer-based CBT-I work?
Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis
Cheng, SK and Dizon, J
Psychotherapy and Psychomatics | June 2012
Abstract
Background: Computerised cognitive behavioural therapy (CCBT) is an innovative mode of delivering services to patients with psychological disorders. The present paper uses a meta-analysis to systematically review and evaluate the effectiveness of CCBT for insomnia (CCBT-I).
Method: A comprehensive search was conducted on 7 databases including MEDLINE, PsycINFO, EMBASE, CINAHL, Cochrane Library, Social Sciences Citation Index and PubMed (up to March 2011). Search terms covered 3 concepts: (1) [internet, web, online, computer-aided, computer-assisted, computer-guided, computerized OR computerised] AND (2) [CBT, cognitive therapy, behavio(u)ral therapy OR behavio(u)r therapy] AND (3) [insomnia, sleep disorders OR sleeping problem].
Results: 533 potentially relevant papers were identified, and 6 randomised controlled trials (RCTs) that met the selection criteria were included in the review and analysis. Two RCTs were done by the same group of investigators (Ritterband and colleagues) using the same internet programmes. Post-treatment mean differences between groups showed that the effects of CCBT-I on sleep quality, sleep efficiency, the number of awakenings, sleep onset latency and the Insomnia Severity Index were significant, ranging from small to large effect sizes. However, effects on wake time after sleep onset, total sleep time and time in bed were non-significant. On average, the number needed to treat was 3.59. The treatment adherence rate for CCBT-I was high (78%).
Conclusion: The results lend support to CCBT as a mildly to moderately effective self-help therapy in the short run for insomnia. CCBT-I can be an acceptable form of low-intensity treatment in the stepped care model for insomnia.
Best complementary health approaches
The National Center for Compelementary and Intregrative Health, a National Institute of Health (NIH), clearly states what IS and IS NOT proven to help insomnia on this page. Briefly, they cover:
- Mind/Body techniques, such as: relaxation, meditation, hypnotherapy, yoga, and acupuncture.
- Supplements, such as: melatonin, chamomile, cava, valerian, L-Trytophan, 5-HTP, lemon balm, passionflower, or hops.
- Other remedies, such as: Aromatherapy, Homeopathic medicine.
Measuring activity while asleep
Practice Parameters for the Use of Actigraphy in the Assessment of Sleep and Sleep Disorders: An Update for 2007
American Academy of Sleep Medicine | April 2007
Measure the Quality of your Care
Measurement of Quality to Improve Care in Sleep Medicine
Timothy Morgenthaler, MD et al
Journal of Clinical Sleep Medicine | Volume 12 Number 8
Abstract
The Board of Directors of the American Academy of Sleep Medicine (AASM) commissioned a Task Force to develop quality measures as part of its strategic plan to promote high quality patient-centered care. Among many potential dimensions of quality, the AASM requested Workgroups to develop outcome and process measures to aid in evaluating the quality of care of five common sleep disorders: restless legs syndrome, insomnia, narcolepsy, obstructive sleep apnea in adults, and obstructive sleep apnea in children. This paper describes the rationale, background, general methods development, and considerations in implementation for these sleep disorder quality measures.
The Workgroup papers are published in this issue under the following titles: Quality Measures for the Care of Adult Patients with Restless Legs Syndrome, Quality Measures for the Care of Patients with Insomnia, Quality Measures for the Care of Patients with Narcolepsy, Quality Measures for the Care of Adult Patients with Obstructive Sleep Apnea, and Quality Measures for the Care of Pediatric Patients with Obstructive Sleep Apnea.