Summary
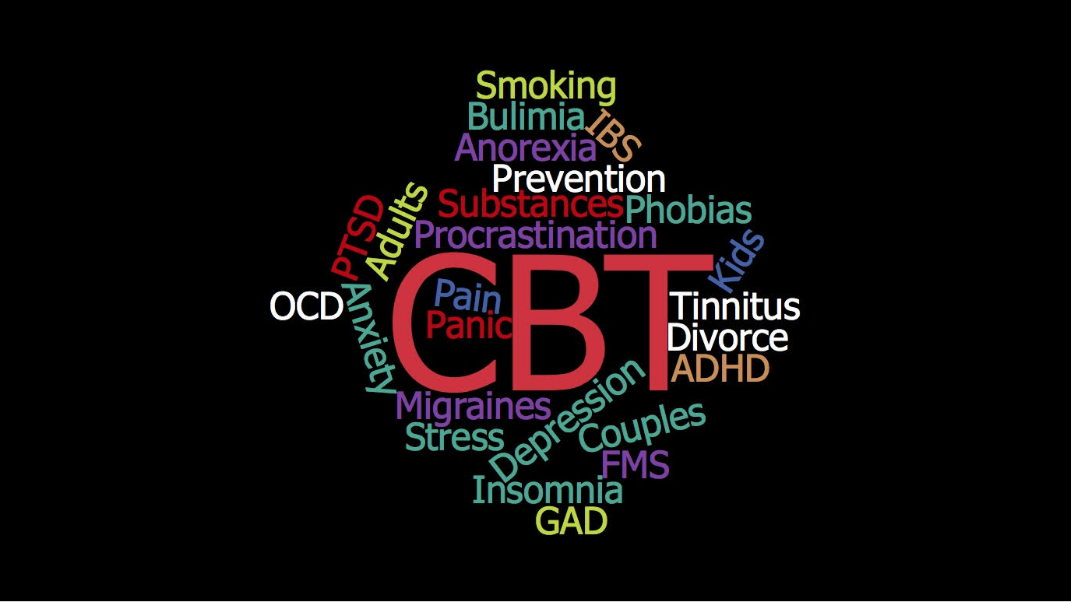
CBT works to change our thoughts and behaviors, which in turn help to change our moods. Although it began with Depression, literally 100’s of clinical trials have shown VERY strong evidence for CBT as a highly effective treatment for the below-listed issues.
OnAir Post: CBT Works!
About
Overview of CBT
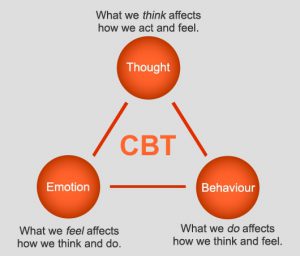 CBT is based on Dr. Aaron Beck’s theory that our automatic thoughts about situations largely influence how we react – emotionally, physically, and behaviorally. Sometimes those automatic thoughts are not exactly true, but we act as if they are. In CBT, people learn to be mindful in the moment and identify what’s true and what’s not. Usually, this results in significantly decreased distress.
CBT is based on Dr. Aaron Beck’s theory that our automatic thoughts about situations largely influence how we react – emotionally, physically, and behaviorally. Sometimes those automatic thoughts are not exactly true, but we act as if they are. In CBT, people learn to be mindful in the moment and identify what’s true and what’s not. Usually, this results in significantly decreased distress.
Often when we behave in self-defeating patterns, automatic thoughts are fueled by automatic beliefs (about ourselves, others, & the world) that aren’t exactly true either. In CBT, when people modify their underlying beliefs (to be more accurate), they’re even able to change lifelong disturbing characteristic ways of behaving.
The goal is to teach people to learn how to identify, evaluate, and modify these patterns themselves. That’s why CBT can be relatively brief, compared to traditional therapies. People can learn to be their own best therapist.
CBT works for …
Adults
- Anger
- Anxiety
- Agoraphobia and Panic Disorder with Agoraphobia
- Dental Phobia
- Generalized Anxiety Disorder
- Geriatric Anxiety
- Obsessive-Compulsive Disorder
- Panic Disorder
- Posttraumatic Stress Disorder (PTSD)
- Social Anxiety / Social Phobia
- Withdrawal from Anti-Anxiety Medications
- Attention Deficit Disorder
- Atypical sexual practices/sex offenders
- Bipolar Disorder (in combination with medication)
- Body Dysmorphic Disorder
- Borderline Personality Disorder
- Caregiver distress
- Depression
- Geriatric Depression
- Relapse Prevention
- Dissociative Disorders
- Eating Disorders
- Anorexia
- Binge-eating Disorder
- Bulimia
- Gambling (in combination with medication)
- Habit disorders
- Marital discord
- Schizophrenia (in combination with medication)
- Seasonal Affective Disorder
- Somatization Disorder
- Substance Abuse
- Alcohol abuse
- Cocaine abuse (CBT relapse prevention is effective)
- Opiate dependence
- Smoking cessation (Group CBT is effective, as well as CBT that has multiple treatment components in combination with relapse prevention)
- Suicide attempts
Medically-related Issues
- Asthma with Coexisting Panic Disorder (in combination with asthma education)
- Cancer pain
- Chronic back pain
- Chronic fatigue syndrome
- Chronic pain (CBT, in combination with physical therapy, is effective for chronic pain in many medical conditions)
- Colitis
- Erectile dysfunction (CBT is effective for reducing sexual anxiety and improving communication)
- Fatigue and functional impairments among cancer survivors
- Fibromyalgia
- Geriatric sleep disorders
- Gulf War Syndrome
- Hypertension (CBT is effective as an adjunctive treatment)
- Hypochondriasis, or the unsubstantiated belief that one has a serious medical condition
- Infertility (anovulation)
- Insomnia
- Irritable-bowel syndrome
- Migraine headaches
- Non-cardiac chest pain
- Obesity (CBT is effective in combination with hypnosis)
- Pain with no known cause (Idiopathic pain)
- Physical complaints not explained by a medical condition (Somatoform disorders)
- Pre-menstrual syndrome
- Rheumatic disease pain (CBT that has multiple treatment components is effective)
- Sickle cell disease pain (CBT that has multiple treatment components is effective)
- Sleep disorders
- Somatization Disorder
- Temporomandibular Disorder pain
- Tinnitus
- Vulvodynia
Children & Adolescents
- Anxiety disorders
- Avoidant disorder
- Chronic pain
- Conduct disorder (oppositional defiant disorder)
- Depression (among adolescents and depressive symptoms among children)
- Distress due to medical procedures (mainly for cancer)
- Obsessive-compulsive disorder
- Overanxious disorder
- Phobias
- Physical complaints not explained by a medical condition (Somatoform disorders)
- Posttraumatic stress disorder
- Recurrent abdominal pain
- Separation anxiety
Other issues
- Aging
- Family therapy
- Grief and loss
- Group therapy
- Low self-esteem
- Psychiatric Inpatients
- Relationship difficulties
- Separation and Divorce
- Stress
- Work problems & procrastination
* Quoted from The Beck Institute (http://www.beckinstitute.org/cognitive-therapy-can-treat/)