Summary
Pain, in the U.S., is the most common complaint in healthcare and an enormous public health challenge. One in 3 adults have it. It causes the most disability. It costs us up to $635 billion/year. By far, pain is untreated or under-treated.
OnAir Post: Chronic Back Pain
About
The National Problem of Pain
Dr. Mackey is Chief of Stanford’s Division of Pain Medicine, Director of the Systems Neuroscience and Pain Laboratory (SNAPL) and Redlich Professor of Anesthesiology, Perioperative and Pain Medicine, Neurosciences and (by courtesy) Neurology.
In this video, Dr. Mackey kicks off the 2016 Back Pain Day by discussing pain as a chronic disease itself and a how we can address it clinically and as a public health problem. He broadly describes what’s involved in pain management – a team sport. Then, the other 8 Pain Medicine faculty members describe their roles on the pain team in their videos.
Sean Mackey, M.D., Ph.D
Dr. Mackey explains, in terms patients can understand, the state-of-the-art understanding about how pain actually works.
aBeth Darnall, PhD
Clinical Professor in the Department of Anesthesiology, Perioperative and Pain Medicine, Dr. Darnall is a pain psychologist and scientist. Her research investigates how to best treat and prevent chronic pain. She is a principal investigator for $14M in federal research awards.
Dr. Darnall explains the importance of using CBT to manage ‘catastrophizing’ – a common reaction to chronic pain.
Heather Poupore-King, PhD
Clinical Assistant Professor, Anesthesiology, Perioperative and Pain Medicine, Dr. King’s interest is in providing interdisciplinary care and specializes in comprehensive functional rehabilitation for chronic pain patients, using Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (a form of CBT), and Biofeedback.
Dr. King explains how care team members work together – with you at the center – to manage chronic pain best.
Fiona Barwick, PhD
Clinical Assistant Professor in Psychiatry & Behavioral Sciences – Stanford Center for Sleep Sciences and Medicine, Dr. Barwick specializes in the assessment and treatment of insomnia, sleep apnea, circadian rhythm sleep-wake disorders, and parasomnias from a Health Psychology perspective.
Dr. Barwick explains the role of CBT and augmented therapies for addressing problems with sleep and chronic pain.
Ming-Chih Kao, MD, PhD
Clinic Chief at Stanford Pain Management and Clinical Assistant Professor, Orthopaedic Surgery, Dr. Kao’s mission is to offer all of his patients comprehensive interdisciplinary diagnosis and treatment, leveraging the full extent of what is known in state-of-the-art Pain Medicine.
Dr. Kao discusses the variety of meds used and their role in pain management.
Michael S. Leong, MD
Clinical Associate Professor of Anesthesiology and Pain Medicine and Neurosurgery (by courtesy), Dr. Leong’s clinical foci are in radiculopathy; spinal, abdominal, and cancer pain; postherpetic neuralgia; and workers compensation cases.
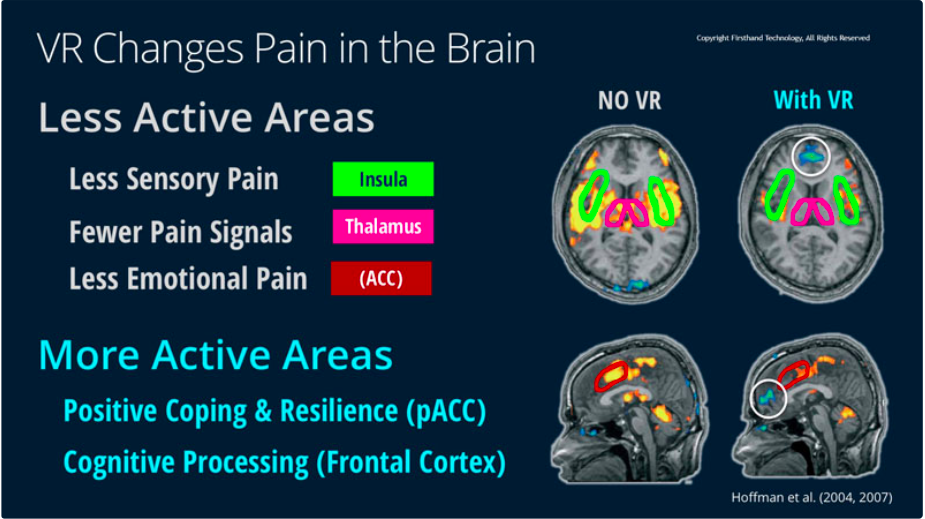
Dr. Leong explains the role of the use of spinal cord stimulation and how it works to reduce chronic pain.
Jordan Newmark, MD
Dr. Newmark is the pain division’s Associate Division Chief of Education, and Pain Medicine Associate Fellowship Director. His clincal interests are in chronic and perioperative pain management, headache and orofacial pain management, and interdisciplinary / procedural treatment.
Dr. Newmark teaches us about the safe use of opioids for chronic pain.
Corinne Cooley, DPT
Ms. Cooley, a member of the Pain Physical Therapy staff, explains the role of physical movement in managing chronic pain – “Movement as Medicine”
J. Drew Sturgeon, PhD
A Postdoctoral Research Fellow, Dr. Sturgeon explains the importance of managing social relationships and shows their impact on the brain and on chronic pain.
Questions and Answers (Video 1 and 2)
The entire panel participates.
The Future: ‘Personalized’ Pain Management
This video, not part of the 2016 Pain Day, outlines how the Stanford team is developing an extraordinary diagnostic and treatment tool that will inform clinicians (throughout the world) how to better ‘personalize’ pain treatment for their patients. Perhaps your physician could participate with this project, CHOIR, in the future.